Statement of Michael J. Astrue
Commissioner of Social Security
Before the Senate Homeland Security and Government Affairs Committee
Permanent Subcommittee on Investigations
August 4, 2010
Introduction
Chairman Levin, Ranking Member Coburn, and Members of the Subcommittee:
Thank you for this opportunity to discuss issues raised in the recent Government Accountability Office (GAO) report, “Cases of Federal Employees and Transportation Drivers and Owners who Fraudulently and/or Improperly Received Social Security Administration (SSA) Disability Payments.” As you know, fighting fraud and improper payments are one of the Administration’s government-wide financial management efforts. At SSA, we are committed to continuing to improve our use of cost-effective methods to prevent, detect, and recover disability overpayments, as well as reduce fraud, and we appreciate your interest in this very important subject.
We recognize that the American public depends on us to be outstanding stewards of the Social Security trust funds. We pay benefits to about 58 million beneficiaries who deserve to receive timely and accurate benefits, and in nearly all of the cases we do. We believe the incidence of fraud in our programs is exceptionally low, and we take great pains to train our field employees in fraud detection and enforcement.
We work diligently to implement complex laws designed to encourage disability beneficiaries to return to work. Accordingly, receipt of both a disability benefit and earnings is not necessarily fraud, and it is not even necessarily an improper payment. A beneficiary who has reported earnings creates a complex question we must answer – namely, are they still eligible for the benefit – and not conclusive proof for a termination of benefits. The complexity increases exponentially when a person receives benefits under the different return-to-work rules of our disability programs.
Earlier this decade, we encountered several years where the Congress appropriated less than the President’s Budget, and our administrative infrastructure contracted to a point where we could not fulfill all of our responsibilities. During this time period, hearing backlogs rose dramatically and program integrity work declined dramatically. Since 2007, we have made significant progress toward reversing these trends, but we still lack the resources to perform all of our program integrity work on a timely basis. GAO itself stated in 2008 that our “service…is still being provided, and mostly in a timely way, but it is extremely fragile.”1 Despite rising workloads, contrary to the impression created by the GAO report, we have been steadily increasing our program integrity efforts and that increase has been accelerating with the support we have received from Congress and President Obama.
The most significant data we have to identify potential improper payments are Internal Revenue Service (IRS) wage reports. Annual reporting combined with the complexity of reviewing these cases create a long lag period between lapsed entitlement to benefits and enforcement. Quarterly wage reporting would improve the timeliness of our program integrity efforts and thus reduce the size of overpayments.
Program Background
The Social Security insurance programs, which include Old Age, Survivors, and Disability Insurance (OASDI) benefits, protect against loss of earnings due to retirement, death, and disability. Social Security benefits are financed through payroll taxes paid by workers, their employers, and self-employed persons. The Supplemental Security Income (SSI) program, funded by general revenues, assists aged, blind, and disabled persons with limited means.
During fiscal years (FY) 2005-2009, we paid over $2.4 trillion to retirement and survivors beneficiaries. In that same period, we paid $490.6 billion to Social Security Disability Insurance (SSDI) beneficiaries and $218.6 billion to SSI recipients.
The definition of disability for SSDI and SSI is unique—we pay only those claimants who are totally disabled and cannot work in any job in the national economy. We do not award SSDI or SSI for partial or short-term disability.
Under the Social Security Act (Act) and our regulations, we find claimants disabled only if:
- They cannot perform their previous work;
- They cannot adjust to other work because of their medical condition(s); and
- Their disability has lasted or is expected to last for at least one year or to result in death.
Furthermore, under the Act, we cannot terminate a beneficiary’s benefits for medical reasons unless we can document medical improvement.
In FY 2009, 99.63 percent of all OASDI payments were free of an overpayment, and 99.91 percent were free of an underpayment. In the SSI program, 91.6 percent of all payments were free of an overpayment, and 98.4 percent were free of an underpayment. While our SSI overpayment rate has improved over the last year and a half, it is still short of an appropriate level.
Issues Raised in the GAO Report
An improper payment does not equal fraud. In its recent report, GAO began its investigation by identifying about 1,500 Federal employees, 62,000 individuals with commercial driver’s licenses (CDL), and 7,900 individuals who registered a commercial vehicle company—all of whom were disability beneficiaries or recipients whose cases had indicators of potential improper payments. Of the 20 cases that GAO reviewed, GAO investigated only one problematic CDL case and only one problematic case involving a commercial vehicle company. GAO did not conclusively prove fraud in any of these 20 cases and has referred only 5 of these cases to our Office of the Inspector General (OIG).
We do not intend to minimize the importance of the issues raised in this investigation, and we take our stewardship responsibilities very seriously. Nevertheless, the results apply to only these 20 non-representative cases, and after reviewing these 20 cases, we found that we had already detected overpayments for half and believe that we would have identified the remaining cases through subsequent enforcement activities if earnings were reported on the W-2 or as self-employment income to the IRS.
We also continue to work collaboratively to combat fraud with the SSA OIG, which has the agency lead for investigating cases of possible fraud. The OIG is set up to efficiently conduct independent and objective audits, evaluations, and investigations, to promote the integrity and security of our programs and operations and protect them against fraud, waste, and abuse.
We have worked with the SSA OIG to establish investigative units—called Cooperative Disability Investigations (CDI) units—across the country. Each unit consists of an OIG special agent, state or local law enforcement investigators, state disability determination services (DDS) examiners/analysts, and SSA management support specialists or similar SSA employees. This initiative provides greater investigative support to the agency so that we may make decisions on disability claims that are more accurate and timely by resolving questions of possible fraud. The CDI program’s process enhances the potential for identifying and preventing overpayments, as well as denying fraudulent initial applications, by fostering an exchange of information between disability decision-makers and the CDI units. The program also ensures timely investigation and the termination of benefits when we detect fraud during continuing disability reviews (CDR), which are medical or work reevaluations to determine if beneficiaries are still disabled.
CDI units also investigate and support criminal prosecution of doctors, lawyers, and other third parties who commit fraud against the SSDI and SSI disability programs. The results of these investigations may also be presented to Federal and state prosecutors for consideration of criminal or civil prosecution, as well as to the OIG’s Office of Counsel for the possible imposition of civil monetary penalties.
There are currently 21 CDI units operating throughout the United States, with a 22nd unit expected to be operational before the end of this fiscal year. According to our OIG, since the program’s inception in FY 1998 through March 2010, CDI efforts nationwide have resulted in $1.4 billion in savings to our disability programs and $891 million in savings to non-SSA programs, such as Medicare and Medicaid. 2
These monetary achievements are the result of CDI units opening more than 29,900 cases and developing evidence to support approximately 23,100 actions, resulting in a denial, suspension, or termination of disability benefits.
In the area of data matching, the GAO investigators declined to recommend matching with CDL and commercial vehicle company registrant data, and we similarly question the value of using these data to evaluate continuing eligibility for disability when the data do not have specific income records associated with them.
We are already going ahead with matching our agency’s payroll records with disability data so we can get the information earlier than from the enforcement process, and we are considering other GAO recommendations to see if we can improve our processes.
We see some promise in the investigators’ recommendation that we evaluate the feasibility of coordinating our automated process for re-computing monthly disability payments with our enforcement process to identify people who have returned to work. This is a systems functionality that we once had and may reinstitute along with other improvements. For example, we are developing a statistical predictive model that identifies beneficiaries who are at risk of high earnings-related overpayments and plan a field test of this model later this month. This predictive model may help us prioritize our scarce staff resources for our enforcement activities, and we believe that it has the potential to reduce the already small number and amount of work-related overpayments.
To bolster the quality and timeliness of our beneficiary-reported data, we are accelerating our work on two projects that make beneficiaries’ reporting of their wages easier and more efficient. We plan to extend the existing SSI telephone wage reporting process to SSDI beneficiaries. Individuals will be able to report their earnings by telephone either by touch-tone or voice recognition. We also plan to establish a website for disability beneficiaries to report their wages easily and promptly. Based on the results of electronic reporting in the SSI program, we may have similar success in reducing SSDI overpayments due to late reporting of earnings.
In many cases, the complexity of our disability programs leads to overpayments. We strive for continued improvement in this area within the limits permitted by the programmatic structures.
While we understand the focus of today’s hearing is on disability overpayments and fraud, we know from experience that we cannot artificially segregate our stewardship and service missions. We use the same limited resources to complete these workloads. These resources include highly trained employees, as well as their time and the physical and technological capacity needed to complete their work.
The President’s commitment to implement a multi-year plan to increase Government-wide program integrity efforts will bolster our stewardship activities. The President’s FY 2011 Budget includes $38 million in additional resources for two major program integrity efforts for our agency: CDRs and SSI redeterminations, which are reviews of nonmedical factors of eligibility such as income and resources. This FY 2011 level represents a 5 percent increase over the FY 2010 level. In addition, the budget includes funding for us to continue nationwide rollout of our Access to Financial Institutions (AFI) project, which automates the verification of SSI applicants and recipients’ assets held by banks.
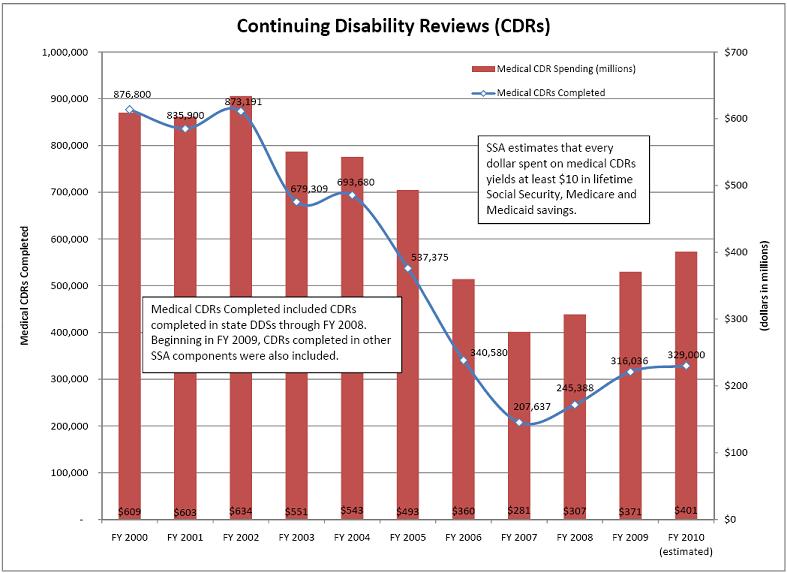
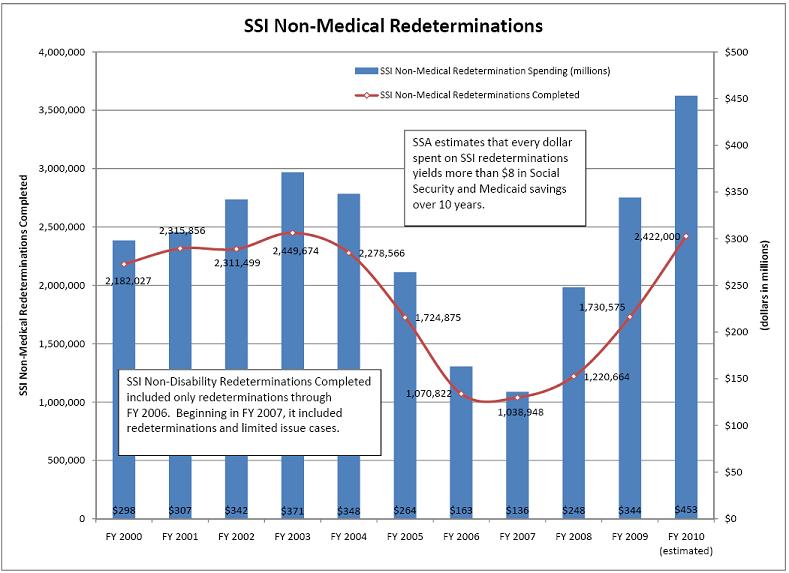
In FY 2011, we plan to conduct 360,000 full medical CDRs and 2,422,000 redeterminations. We estimate that every dollar spent on medical CDRs yields at least $10 in lifetime Social Security, Medicare and Medicaid savings, and every dollar spent on SSI redeterminations yields more than $8 in Social Security and Medicaid savings over 10 years. If we meet our FY 2011 program integrity goals for medical CDRs and redeterminations, the estimated program savings over the 10-year period through FY 2020 amount to more than $7 billion, including Medicare and Medicaid savings.
Understanding the Causes of Disability Overpayments
While the leading cause of SSI overpayments is an unreported increase in financial accounts and wages, the leading cause of overpayments in the SSDI program is error in determining whether a beneficiary is engaging in substantial gainful activity (SGA). Beneficiaries who fail to report work activities are a significant source of errors in calculating SGA. SGA refers to the performance of significant physical or mental activities in work for pay or profit or in work of a type generally performed for pay or profit. SGA is a test for determining both initial and continuing eligibility for SSDI. In all initial claims situations, if a claimant’s work is over SGA, then the claimant does not meet the definition of disability and does not receive benefits.
Generally, countable earnings averaging over $1,000 a month (in 2010) demonstrate the ability to perform SGA. For blind persons, countable earnings averaging over $1,640 a month (in 2010) generally demonstrate SGA for SSDI. These amounts, however, are subject to modifications and exceptions based on statutory incentives designed to encourage work.
Some of the work incentives that we may apply to reduce countable earnings for SSDI are:
|
After an SSDI beneficiary completes the TWP and continues to work, we conduct a work CDR to determine if the beneficiary’s earnings preclude entitlement to payment. We may also receive either a report of earnings or an earnings alert for unreported earnings. Our Continuing Disability Review Enforcement Operation (CDREO) uses IRS earnings data to identify possible work CDRs for SSDI beneficiaries. In all cases, we must provide due process prior to taking any adverse action. Throughout the course of case development, disability beneficiaries may ask us at any time to suspend their benefits if they wish to avoid an overpayment.
For SSI disability, SGA is a test to determine only initial eligibility rather than continuing eligibility. When an SSI disability recipient returns to work, we do not apply SGA. We count income and earnings (after allowable deductions) to determine the monthly payment amount. The countable income is subtracted from the Federal benefit rate ($674 in 2010) to arrive at the payment.3 An SSI disability recipient may go in and out of pay status based on countable income. An SSI recipient whose payment is reduced to zero because of earnings will retain eligibility to SSI and to Medicaid, if the disabling condition continues and earnings are below a state threshold amount. State thresholds vary between an annual low of $23,981 in Alabama to a high of $54,815 in Connecticut.
Some of the work incentives that reduce countable earnings for SSI disability are:
|
Given the complexity of the statutes for our disability programs, some overpayments are unavoidable. The complexity of our work incentive provisions is exacerbated when a beneficiary receives both SSDI and SSI. A simple example of this complexity for such a beneficiary is the fact that the amount of earnings that we count for the same month is often different in each program. For SSDI the earnings are counted for the month that they are earned; for SSI they are counted for the month that they are paid. We are currently exploring ways to simplify our disability programs to reduce overpayments.
Detecting and Preventing Disability Overpayments
“Curbing Improper Payments” is the first objective under our 2008-2013 Agency Strategic Plan Goal to “Preserve the Public’s Trust in Our Programs.” Our primary tools for achieving this objective are CDRs and SSI redeterminations. A work CDR is a review of eligibility requirements regarding an SSDI beneficiary’s earnings or ability to work. Work CDRs are triggered by reports of earnings from beneficiaries or third parties, systems alerts, and earnings posted to a beneficiary’s record. We process work CDRs in field offices and processing centers. We use a program called eWork to automate work CDR processing. eWork collects necessary data from mainframe databases, prepares forms, notices, and work report receipts, incorporates policy and decision logic, and adjusts benefits.
Act requires us to conduct medical CDRs on a periodic basis to evaluate whether disabled beneficiaries and recipients continue to meet the medical criteria. We also conduct medical CDRs when we receive a report of medical improvement from a disability beneficiary or recipient or third party. We complete medical CDRs in two ways. The medical CDR process uses a statistical modeling system that uses data from our records to determine the likelihood that a disabled beneficiary or recipient has improved medically. If the statistical modeling system indicates that the beneficiary or recipient has a high likelihood of medical improvement, we send the case to the state DDS for a full medical review. We send the remaining beneficiaries and recipients a questionnaire requesting updates on their impairments, medical treatment, and work activities. If the completed mailer indicates that there has been potential medical improvement, we send the case to the DDS for a full medical review. Otherwise, we decide based on the mailer response not to initiate a full medical CDR, and we schedule the case for a future review.
We evaluate all of the non-medical factors of SSI eligibility by conducting SSI redeterminations. There are two types of SSI redeterminations: scheduled and unscheduled. We target the most error-prone cases each year using a statistical model. We conduct unscheduled redeterminations when recipients report, or when we discover, certain changes in circumstances that may affect their SSI payment eligibility or amount, such as a change in living arrangements.
Our payment accuracy rate with respect to SSI overpayments has been a challenge, and one we have worked hard to address. In FY 2008, our SSI overpayment accuracy rate was 89.7 percent. To improve our performance, we increased the volume of redeterminations we conducted in FY 2009. Largely as a result of this increase, the overpayment accuracy for 2009 has risen to 91.6 percent, which is a statistically significant improvement over the 2008 rate. Our success in improving the SSI overpayment accuracy rate is encouraging news and demonstrates the value of adequate funding of redeterminations.
In addition to CDRs and redeterminations, we have developed other program integrity initiatives where we use cost-effective means to help us prevent disability overpayments. We continue to roll out our AFI project, which assists us in identifying disclosed and undisclosed financial accounts in the SSI program. The AFI project currently operates in California, New York, and New Jersey. We plan to expand AFI to 14 more states in September, and plan to continue expansion until it is national. We project lifetime program savings of over $100 million in FY 2011 and up to $1 billion in lifetime program savings each year when AFI is fully implemented.
To make it simpler and more convenient for SSI recipients to report wages, last year we implemented an automated monthly telephone wage reporting process. The process uses both touch-tone and voice recognition telephone technology to collect wage reports. Our software automatically enters the wage data into the SSI system, which is much more efficient than if the recipient visited a field office and we manually entered the report into our system. Moreover, telephone wage reports are highly accurate. Based upon a previous study, the dollar accuracy of reported wages using telephone wage reporting was 92.2 percent, compared to the 75.5 percent dollar accuracy of the wage estimates received through other means. We promote use of the telephone wage reporting system, and we provide SSI recipients with training on how to use the system. We are also looking at offering on-line reporting systems.
Technology improves accuracy in multiple ways. Electronic data matching provides a foundation for our ongoing program integrity work, including prevention of disability overpayments. Data matching allows us to obtain information quickly and inexpensively and helps us to automate the process of adjusting or terminating benefits. When deciding what data matches to pursue, we always consider the cost-benefit analysis of those activities, pursuing only those that produce a high return on investment.
Our most important Federal data-matching initiative is our match with IRS annual wage data through CDREO. We also receive income data from IRS for other purposes. For example, we obtain IRS 1099 data for SSI recipients. Cases with IRS amounts over certain tolerance levels are sent to the field offices for review. Some of these cases result in overpayments or ineligibility due to under-reported income. We also use Modified Adjusted Gross Income (MAGI) from IRS to determine Medicare Part B premiums for beneficiaries. The Medicare Modernization Act of 2003 created tiered premiums based on the beneficiary’s MAGI. The MAGI matching operation helps us compute Medicare premiums correctly.
Using our Electronic Death Registration (EDR) process, states electronically transmit death information to us over the Internet so that we quickly receive death notices from the states for OASDI beneficiaries and SSI recipients. As of today, 29 states and jurisdictions have implemented EDR and 9 more states are expected to implement EDR in 2010 or 2011. We currently receive over 36 percent of all death records through EDR. Obtaining these records electronically allows us to update our records more quickly than the traditional reporting process and prevents improper payments after an individual’s death.
We also work with correctional facilities to identify beneficiaries who are incarcerated and should not receive benefits. We currently have agreements with the institutions that house 99 percent of all prisoners in the country. Since 1997, we have suspended benefit payments to approximately 811,000 inmates.
Recovering Disability Overpayments
In addition to our efforts to prevent and detect improper payments, we also aggressively seek to collect debt through a wide-variety of methods. We use both internal and external collection tools to collect what we are owed. The technique we use most widely and most successfully for beneficiaries who continue on the disability rolls is benefit withholding. Subject to statutory constraints, we can withhold some or all of an individual’s benefits. We collected over $2 billion last fiscal year using this method.
When we cannot recover a debt on our own, we turn to authorized external debt collection tools. These tools include:
|
As systems resources permit, we will enhance our debt collection by using offset of state payments, including state tax refunds. We are also making plans to charge administrative fees and interest on debt.
While we do not collect all of the overpayments we make in our programs, we make every effort to recover as much as we can. In FY 2009, we recovered over $3 billion in program debt and, over a five-year period (FYs 2005-2009), we collected $12.75 billion at an administrative cost of $.06 for every dollar collected.
In providing us with these debt collection tools, Congress recognized that maximum debt collection is not the only consideration. Rather, by the terms of the Act, we must balance our stewardship responsibilities with compassionate recognition of our beneficiaries’ individual situations. For example, we are limited to withholding no more than 10 percent of an SSI recipient’s monthly income to recover an overpayment. Reducing the already minimal SSI payment any further would leave the recipient without enough money to meet basic living expenses. Similarly, the Act prohibits recovery of overpayments from any beneficiary who is without fault if the recovery would defeat the purpose of the programs or be against equity and good conscience. In determining if the beneficiary is without fault, we are statutorily required to consider the person’s physical, mental, education, or linguistic limitations.
Although we make every effort to preserve taxpayer dollars, we administer programs that Congress explicitly designed to provide assistance over revenue maximization. Through these restrictions, Congress has struck a balance between maximum collection and recognition of people in economic distress. We implement our programs with both principles in mind.
Conclusion
The programs we administer demand stewardship that is worthy of their promise of economic security from generation to generation. We are firmly committed to sound management practices, including accurate metrics for evaluating our programs’ integrity, and following up with appropriate enforcement and recovery actions. We know the continued success of our programs is inextricably linked to the public’s trust in them. Properly managing our resources and program dollars is critical to that success. Equally important to our success is Congress providing us with adequate and sustained funding to carry out our work.
Full funding under the President’s FY 2011 Budget will allow us to implement the Administration’s plan to increase program integrity over the next several years. For this reason, we ask that you support the critical funding that President Obama has requested for us.
_________________________________________________
1 Statement of Barbara D. Bovbjerg, Director, Education, Workforce, and Income Security, GAO, before the Senate Committee on Finance on May 8, 2008. 2 OIG Spring 2010 Semi-Annual Report to Congress and SSA FY 2009 Performance and Accountability Report, Inspector General Statement on the SSA’s Major Management and Performance Challenges. 3 State thresholds are determined by SSA under a formula using the SSI Federal benefit rate, state supplementary payment amount (if any), and the per capita Medicaid expenditure in the state. If an individual exceeds the state threshold, we look at his or her actual medical expenses to determine continuing Medicaid eligibility.
|